Intrathecal Analgesia Protocols - Morphine Calculations, Pumps, HAS Compliance
Clinical Resources for Intrathecal Analgesia
Evidence-based guidelines derived from SFETD Toolbox 2024 and PACC international recommendations
Educational Resources
These comprehensive guides synthesize clinical information from the SFETD (Société Française d’Étude et de Traitement de la Douleur) Intrathecal Analgesia Toolbox 2024 and international expert consensus guidelines.
Clinical Practice Guidelines
Intrathecal Analgesia Indications
Comprehensive guide to patient selection and clinical indications for intrathecal drug delivery systems:
- Patient selection criteria for cancer and non-cancer pain
- Absolute and relative contraindications based on SFETD guidelines
- Collegial decision-making process and multidisciplinary team composition
- Anatomical considerations for catheter positioning
- Evidence base from French (SFETD, SFAR, HAS) and international sources
Target Audience: Pain management specialists, oncologists, palliative care physicians, anesthesiologists
Intrathecal Drug Protocols
Evidence-based medication protocols for intrathecal analgesia:
- PACC international recommendations (first, second, third-line therapies)
- Morphine dosing guidelines with conversion formulas (oral to IT)
- Local anesthetics (ropivacaine, bupivacaine) for neuropathic pain
- Ziconotide protocols for refractory pain with gradual titration strategies
- Drug combinations and compatibility based on pH and stability data
- Flow rate settings and bolus programming
- Dose adjustment algorithms for insufficient analgesia or adverse effects
Target Audience: Prescribing physicians, clinical pharmacists, pain management nurses
Reference Materials
Medical Terminology Glossary
Comprehensive glossary of intrathecal analgesia terminology:
- Over 80 medical terms defined from SFETD standards
- Acronym quick reference for clinical documentation
- Drug classifications and mechanisms of action
- Pump technology terminology (IDDS, SynchroMed II, myPTM)
- Procedural terms (refill, programming, bolus types)
- Regulatory terminology (HDS, FHIR, CE marking)
Target Audience: Multidisciplinary teams, medical students, healthcare administrators
Evidence Base
These educational resources are synthesized from authoritative sources:
French Guidelines
SFETD Intrathecal Analgesia Toolbox (2024)
- Comprehensive practical handbook developed by expert panel
- Endorsed by SFETD Pain and Cancer Commission
- Covers complete patient pathway from pre-implantation to end-of-life care
HAS Recommendations (2020)
- Official recognition of intrathecal analgesia for refractory cancer pain
- Published by Haute Autorité de Santé (French national health authority)
SFETD/SFAR Formalized Expert Recommendations (2013)
- Joint recommendations from French pain and anesthesia societies
- Established clinical standards for intrathecal therapy in France
DGOS Instruction (2017)
- Direction Générale de l’Offre de Soins official guidance
- Regulatory framework for intrathecal analgesia programs
International Guidelines
Polyanalgesic Consensus Conference (PACC) 2017
- International expert consensus on intrathecal drug delivery
- Evidence-based medication selection and dosing algorithms
- Risk mitigation strategies for safe implementation
Deer TR, Pope JE, Hayek SM, et al. The Polyanalgesic Consensus Conference (PACC): Recommendations for Intrathecal Drug Delivery: Guidance for Improving Safety and Mitigating Risks. Neuromodulation. 2017 Feb;20(2):155-176.
Clinical Context
The Challenge
Approximately 15% of cancer patients experience refractory or intractable pain, particularly in advanced disease stages. According to the SFETD:
“Intrathecal analgesia should be made available in all of France to ensure equal access to care. This objective is still far from being achieved.”
Unfortunately, healthcare professionals are insufficiently informed about intrathecal analgesia potential, and the technique is underutilized despite its demonstrated effectiveness.
The Solution
The SFETD Intrathecal Toolbox provides:
- Practical information for pain teams wishing to develop intrathecal analgesia programs
- Day-to-day practice guidance for implant facilities, initiation centers, and follow-up departments
- Structured workflows adapted to local resources
- Patient pathway organization from pre-implantation through long-term management
Implementation Support
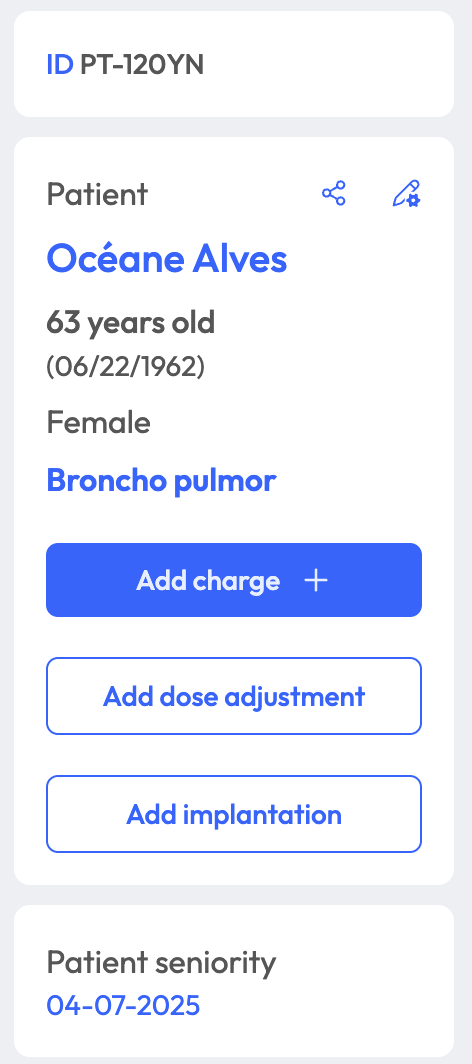
Thalivia digitalizes these evidence-based protocols:
- Structured prescription aligned with SFETD calculator recommendations
- Automated dose calculations using PACC algorithms
- Drug stability monitoring (21-day morphine-ropivacaine-ziconotide protocol)
- Pharmacy integration for ISO 5 cleanroom preparation workflows
- Complete traceability meeting HDS and GDPR requirements
Learn more about Thalivia’s clinical features →
For Healthcare Institutions
Developing Intrathecal Programs
The SFETD Toolbox identifies prior requirements for starting intrathecal therapy:
Team Requirements:
- Motivated physicians trained or amenable to training (minimum 2)
- Dedicated nurses familiar with technique (minimum 2)
- Implanting anesthetist or neurosurgeon
- Coordination (nurse and secretary)
Infrastructure:
- Technical platform for implantation
- Full hospitalization beds for post-operative equilibration
- Day hospital for pump filling and programming
- Mandatory partnership with in-house pharmacy
Pharmacy Capabilities:
- ISO 5 cleanroom (laminar flow hood)
- Dedicated staff with availability
- Drug preparation or dispensing capacity
- Stability expertise for intrathecal mixtures
Administrative Framework:
- Service project validated by relevant authorities
- Collaboration agreements across entities
- 24/7 telephone hotline
- IT tool to secure intrathecal prescribing
Contact Thalivia for institutional implementation support →
Continuing Education
Target Audiences
These resources serve healthcare professionals involved in intrathecal analgesia:
- Pain Management Specialists (algologists)
- Anesthesiologists performing implantations
- Oncologists managing cancer pain
- Palliative Care Physicians treating end-stage disease
- Clinical Pharmacists preparing intrathecal mixtures
- Pain Management Nurses performing refills and patient education
- Hospital Administrators developing pain management programs
Learning Objectives
After reviewing these resources, clinicians will understand:
- Patient Selection: Indications, contraindications, and collegial decision-making processes
- Medication Protocols: PACC-aligned drug selection, dosing calculations, and titration strategies
- Safety Protocols: Complication prevention, adverse effect management, and error reduction
- Technical Procedures: Pump implantation, refilling techniques, and programming workflows
- Organizational Requirements: Team structure, pharmacy integration, and regulatory compliance
Evidence-Based Practice
Thalivia supports implementation of these evidence-based guidelines through:
Clinical Decision Support:
- Automated morphine conversion (oral/IV to intrathecal)
- Local anesthetic dosing by catheter level (cervical vs. thoracic)
- Ziconotide titration recommendations (0.1-0.2 µg/24h increments)
Safety Features:
- Maximum dose limits (e.g., morphine ≤5 mg/24h initially)
- Flow rate validation (typical start: 1 mL/day IDDS)
- Bolus parameter checks (refractory period, max activations)
- Drug stability tracking (21-day MRZ mixture limit)
Workflow Integration:
- Pharmacy collaboration per SFETD circuit recommendations
- Collegial decision documentation
- Complete audit trail for regulatory compliance
- FHIR/HL7 interoperability with EMR systems
Book a demo to see SFETD protocols in action →
Additional Resources
External Links
- SFETD Official Website
- SFETD Toolbox IT (PDF)
- HAS Recommendations (2020)
- Medtronic SynchroMed II Technical Information
Thalivia Platform
- Smart Intrathecal Prescription Features
- Clinical Collaboration Tools
- Product Roadmap
- Frequently Asked Questions